If COVID-19 was the earthquake, digital transformation were the tremors that followed.
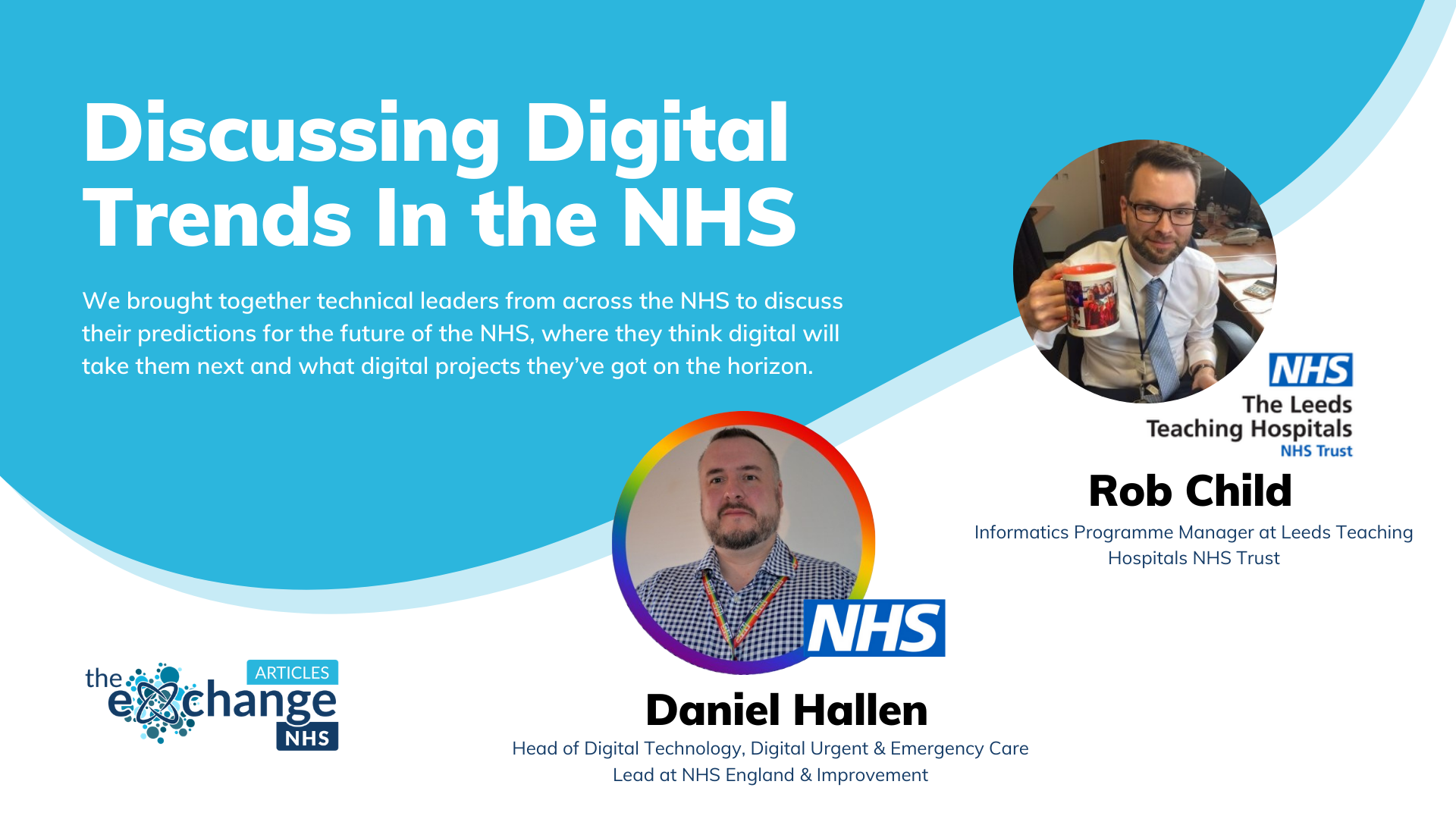
What does the future hold for NHS digital? We brought together technical leaders from across the NHS to discuss their predictions for the future of the NHS, where they think digital will take them next and what digital projects they’ve got on the horizon.
Starting his career as an analyst at a Primary Care Group, Rob moved to the LEA’s Health Authority. After they were disbanded and turned into Primary Care Trusts, Rob joined Leeds Teaching Hospital in 2006 on what was then known as the Trans4orm Programme which aimed at creating efficiencies and reducing costs through the delivery of number of projects.
After that, Rob became an Information Manager within Digital IT (DIT), but then in 2012, got an opportunity to manage the Transforming Outpatients Programme. Focusing on consolidating outpatients into a central function, Rob’s progressive digital transformation work allowed him to step into DIT Programme Management, leading the Programmes & Projects and DIT Project Delivery Office.
We all have ideas and opinions on how the processes we work with can be improved – but we don’t always know where to take them and how to articulate them.
In an institution the size of the NHS, with larger silos in the form of the individual Trusts, you have an even bigger challenge to find a way to harness the ideas of those who work with the systems and break those ideas down into projects that can be executed.
DIT’s solution comes in the form of the new Project Delivery Lifecycle (PDLC). This is designed to improve the process for implementing new ideas by bringing them through a three-step process – first assessing viability and the challenges before proceeding to a project initiation stage.
Going from project initiation, define and plan, launch and execution, acceptance in service cutover, and then project closure, the process that has been created is a very clear way of taking ideas and running projects.
“There’s a lot of demand for digital solutions at Leeds. But it’s a really good thing because people can see their ideas being taken seriously and we get a flavour for the digital appetite of the Trust.”
Rob and his team are at the tip of the spear when it comes to digital trends in an NHS setting.
COVID has only highlighted the fact that many NHS trusts have been neglected for a very long time. There are many old buildings, with old infrastructure that cannot keep up with the pace of change the NHS, as an institution, demands.
And now that everyone has proven that they can work effectively while remote, it’s a question of when the investment is coming and not if.
“COVID just gave it a shot in the arm. We had to upscale our VPN, and also provide extra equipment to support people to work from home. .
“How are we going to blend those two worlds? Are we going to need less offices? More cameras? It’s a challenge we’re going to have to work our way through because there is no one-size-fits-all.”
With new models of care emerging and evolving, there is a clear need for more effective information sharing between care settings, organisations and geographies, as well as between professionals and citizens, to optimise patient outcomes and quality of care.
Interoperability and integrated care was very much the direction that the NHS was moving in with the introduction of nearly 30 ICS over the past few years. Enabling health and care organisations to join forces and apply their collective strength to addressing their residents’ biggest health challenges, interoperability was another development highlighted by the COVID-19 pandemic.
The less people and items in the chain of care, the better.
“We’ve recently done some work with Point of care devices that communicate with our EHR. We’ve got COVID and Flu analysers hooked up and we’ve got a whole neonatal department that wants to hook up their devices to communicate with the same system.”
It’s been reported heavily recently that the waiting list for surgeries in England is now the longest since records began. The question on the lips of NHS professionals now is: ‘Who needs to be coming back into hospital?’
“There’s been a big drive around patient-initiated follow ups. We’re not going to tell you when to come, you tell us when you need to come. So we’re breaking that six month cycle where people turn up just to tell us that they’re fine.”
Daniel Hallen is the Head of Digital Technology and Digital Urgent & Emergency Care at NHS England & Improvement (North West). With responsibility over anything digital in his ICS footprints, as part of the NHS England & Improvement regional team, Daniel and his colleagues act as the oversight and tempo setter for digital strategy.
With a mix of public and private sector experience in programme management, Daniel brings a variety of skills to his role. Initially studying Law , Daniel chose a different direction for his career and hasn’t looked back.
“We’re driven very much around how we do things better not just for our patients, but for our staff as well. Because it’s all well and good introducing a clinical digital system that is really good for our patients, but it’s got to be effective for our staff. So trying to improve things as we go along. But also us taking lots of lived experience of people, that myself included as a patient to improve the systems that we have out there.”
Organisations around the world spent a lot of money and resources over the last 12 months on agile digital solutions in response to the COVID-19 pandemic. The NHS is no different and the benefits of that investment are there for all to see.
Less people coming into hospital, less children being taken out of school, less CO2 being produced on needless journeys. Car parking costs are down. Clinician time is optimised.
With all those benefits, the question now becomes: how do we keep that going? A good starting point, for Daniel, is having serious, and sometimes difficult, infrastructure rationalisation discussions.
“Does everyone need a laptop? Does every trust need a data centre? We need to be more creative and collaborative with our solutions now that we’re starting with Integrated Care Services. Why can’t we drop data centers into the ocean like Microsoft?”
The NHS is a multi-billion pound organisation that is driven by people within it. The Clinicians and the nurses don’t catch as many headlines as the breakthrough technology that the NHS is using to improve the service, but they are the most important aspect of care.
For Daniel, investment in their people mustn’t be left behind by investment in the technology.
“It doesn’t matter what technology you create, it’s the people’s time that actually puts it in place. So it’s the people part of the digital transformation which is the important bit.”
One way that Daniel is ensuring the people-aspect of digital transformation is considered is by studying the organisations around the world who continue to break new ground in the digital space – with his spare eye always on the people who would be tasked with driving this technology throughout the NHS.
“I love technology, it’s the core of what I do. But if you don’t empower people, nothing changes. And that’s what’s really been shown this last 15 months, it’s been all about people.”